BPD episodes are hard to live with when you have the condition. Teens with BPD do not have it easy. Parenting a teen with BPD can be complicated too. BPD episodes can be difficult to manage as a parent of a borderline teenager. I know firsthand because I am in remission from borderline personality disorder after over a decade of mental health treatment. I also have a teen who has many BPD traits (but is still too young to be formally diagnosed), which makes sense because BPD runs in our family.
The following post lays out what I would have wanted done for me, as a teen with BPD, and is what I keep in mind for my son whenever he’s in an intense emotional state of his own. It takes time and patience to get the hang of and things will never be 100%, but these steps work for us. On top of de-escalating intense emotions, they strengthen our relationship and build up my son’s mental wellbeing too.
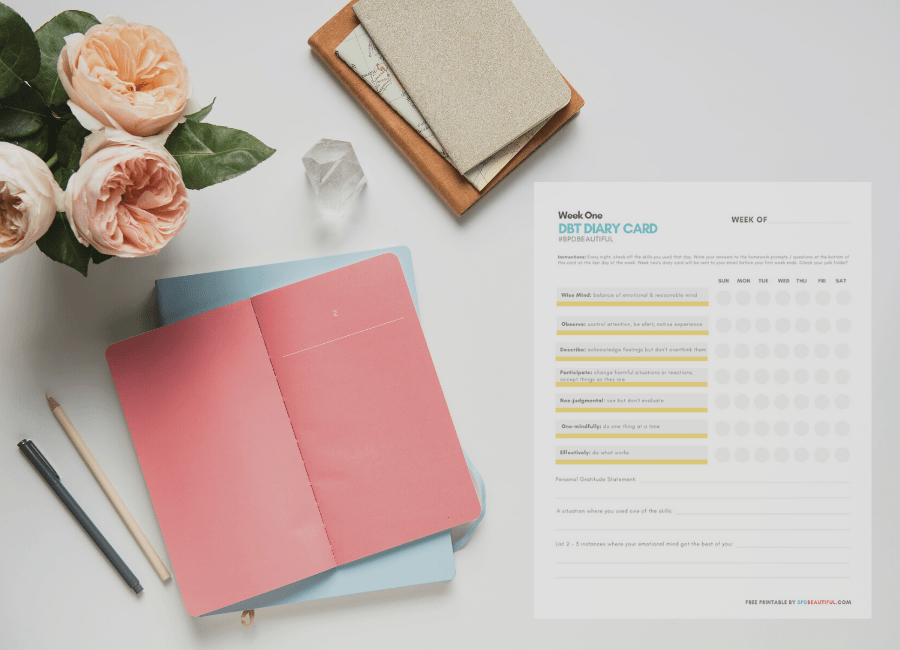
Side note: It’s also immensely helpful to learn, understand and practice healthy coping skills (like DBT’s emotional regulation module) yourself—so you can be a good role model for your borderline teenager. More on that later on in this post.
Keep in mind, I use terms like “borderline teenager” or “teens with BPD” in this post for search engine purposes. But while out in the ‘real world’ or communicating with others (especially your teen), we should refrain from labeling people as their condition like this. “She’s BPD” does not make grammatical sense, anyway. Those of us with borderline personality disorder are so much more than our diagnosis and labeling people like this only adds to the BPD stigma.
Signs of BPD in a Teenager
Before we get to the root of this post, let’s first go over some signs of BPD in a teenager in case you’re still waiting to hear back from a professional on a diagnosis or are wondering if it’s time for an evaluation. Honestly, these are the same signs one would likely see in an adult with BPD as well.
(Read ‘What Happens During a BPD Episode’)
Please note that these signs are not set in stone (everyone is different) and they cannot be used as a way to diagnose others. What may look like BPD, could actually be something else which is why having a professional’s input is essential.
Signs of BPD in a teenager are…
- They become hyper focused on and are possibly obsessive over one particular person. For the case of a teen—this is typically a best friend, crush or romantic partner but it could also be a teacher, parent, family member or someone else. You may notice they talk about this person A LOT, look up & idealize them (see them as perfect), get anxious when they’re not around or change their opinions or preferences to match theirs. This “favorite person” likely changes over time and may change suddenly. It can even be a celebrity. I personally had a celebrity “favorite person” when I was a teen but usually, it was whoever I was in a relationship with.
- They frequently display extreme, black & white or all or nothing thinking. This is typically displayed in their words, especially during (possible) BPD episodes, but it can also come to light through their actions and opinions. They typically switch back and forth from idealizing people, things, beliefs and themselves to devaluing them. This is referred to as “BPD splitting.”
(Read ‘What a Devaluing Split Looks Like for Borderline Personality Disorder‘) - They have frequent and incredibly intense mood swings. These moods can appear to be much more intense than an average teenagers’ that are solely influenced by hormones and developing brains. When triggered, teens with BPD can go from 0-100 and go from raging to being apologetic to being despondent within seconds or minutes. These mood swings often do not last longer than a day or so.
- They have frequent suicidal ideation and/or attempts. Suicidal ideation that’s influenced by BPD is typically a result of interpersonal conflicts or miscommunications as opposed to depression alone (although depression is also common in those who have BPD). These teens may need to be hospitalized often. Personally, I spent a lot of my teenage years in and out of psychiatric hospitals.
- They may have a chronic and dangerous habit of self mutilation or self destructiveness. A lot of people with BPD, myself included, have a history of cutting themselves and are impulsive. This symptom of mine started when I was as young as 11 years old.
- They have an ingrained and overwhelming fear of abandonment. This could appear as separation anxiety or be much more subtle. It’s most likely displayed in their relationship with their “favorite person” mentioned above but can come out with everyone they’re close with. Some people with BPD, including teens, hide this symptom very well—because it usually induces lots of shame and embarrassment. Instead of voicing their fears, teens with BPD may become irritable or agitated when their fear of abandonment has been triggered. They may take it out on you or other family members. They may mask it by starting fights over unrelated situations, or they may withdraw themselves from interpersonal settings.
These are not the 9 symptoms of BPD verbatim, but they are common traits. If you’re not sure if your teen has BPD but you realize they have traits, you should definitely get them evaluated by a psychiatrist. Getting a diagnosis earlier in life will increase your teen’s chances of success and can help them lead fulfilling, satisfying lives faster—contrary to outdated medical beliefs, BPD is treatable. Many others are in remission just like me. A BPD diagnosis does not have to be a death sentence.
Keep in mind, that most mental health professionals will not diagnose a teen with BPD if they’re under 16 and some, even later than that. Regardless of whether they have a formal BPD diagnosis or not, the tips in this post can still help if your teen is highly sensitive or just has traits of BPD without meeting diagnostic criteria.
“READING [SADIE’S FAVORITE] IS AN EMOTIONAL ROLLERCOASTER.” -BETA READER
Sadie’s Favorite by BPD Beautiful creator Sarah Rose is a novel that tells the story of a girl lost, a woman recovered and the trauma in between.
Steps to De-Escalate BPD Episodes in Borderline Teenagers
Without further ado, here are my tips on managing BPD episodes or episodes of intense emotional reactions for parents of teens with BPD or for parents of highly sensitive teens.
For search engine purposes (to reach a broader audience and raise awareness), I will continue using terms like “BPD episode” or “teens with BPD” throughout this post even though your teen may not actually have or be diagnosed with borderline personality disorder. Be careful not to diagnose others yourself. Only a professional can do that.
- Always keep in mind: Reasonable consequences, boundary enforcement, apologies, making amends and open communication can come AFTER the BPD episode has been de-escalated (when teens with BPD will be much more receptive to it). The last bullet point in this post goes over this in more detail.
- When your borderline teenager is in an intense emotional state or when their emotions are quickly rising—listen actively and/or focus on their emotions. Try not to focus on their words or actions during this time. As hard as it is, put your own feelings aside for the duration of the BPD episode so you can help them self-regulate. During intense emotions, it’s unlikely they’ll be able to think about anything else but how they’re feeling. That’s why you should hold off on enforcing boundaries or respectful behavior or speaking of consequences until after things have settled down.
- Don’t allow yourself to become defensive to false accusations or claims, stay as calm and as monotone as naturally possible. Don’t argue back or take their (possibly extreme and hurtful) words to heart. If you feel your own emotions rising at any point, tell them “I’m not in a mindset to be able to handle this / talk about this right now. I need a few minutes / a couple of hours to collect my thoughts. We can talk after. I promise I will be willing to hear you out once I’ve calmed down.”
- Validate their concerns and pushbacks by being willing to hear out their opinions. This doesn’t mean you have to agree with them or condone disrespectful behavior, just give them the time to express what they’re feeling, thinking or looking for so they have a chance to regulate their emotions and calm themselves down.
- Your teen with BPD likely will have difficulty expressing their feelings through effective words and may instead act on them destructively or by saying impulsive & hurtful things that they don’t truly mean. This is especially true if they’re argued with or feel dismissed—which is why keeping your own emotions in check is so important. If they’re acting destructively or impulsively, remain calm and ride out the storm to the best of your ability. Keep a close, discreet eye on them if you’re worried they’ll do something harmful to themselves. Model your own emotional regulation by deep breathing, counting down slowly & quietly from 10 or by using other DBT emotion regulation skills.
- Don’t attempt to talk them out of their feelings or try to convince them how or why they’re wrong, as this can feel dismissive which will only further escalate intense emotions. Do not tell them how they should be feeling or what they should do while they’re in a high emotional state or crisis. Correction or discipline can come AFTER their emotions have calmed down.
- Remain silent while remaining interested and concerned in what they’re expressing. Ask questions to convey your interest while not necessarily conveying agreement. For example, you could ask things like: “How long have you felt this way?” or “What’s happened that triggered these feelings?” or “What’s made you think this way?”
- If there is some truth in what you’re hearing when they express themselves, be open to admitting it out loud to them. Model to them what it means to take accountability as this also teaches them empathy. You can say something along the lines of “I’m sorry. I didn’t mean to make you feel _____. I will try to be more ________ going forward. I love you, and I want there to be MUTUAL respect between us. You are so important to me, and so is our relationship. Please know that you are free to come to me with your concerns in the future, as well. Your opinions matter too.”
- After your teen with BPD has expressed their feelings—make statements that express what you think you’ve heard from them. Allow them the chance to clarify if your interpretation is off. This is validating and can help further de-escalate things. Empathetic, validating statements do NOT need to imply agreement or be condoning of bad behavior. For example, you could say things like:
- “You feel like I don’t love you / I’m not listening?”
- “You’re saying you feel frustrated / angry / disappointed.”
- “You feel (or it seemed like you felt, if they refused to express their feelings – see below) disappointed / unheard / shamed / embarrassed?”
- “It makes sense you would feel _____, if my assumptions are correct and that’s the case.”
- “I understand you feel frustrated. I would feel the same.” (say only if true)
- “I can relate to that.” (say only if you actually can)
- “That can be really hurtful / embarrassing / upsetting / disappointing.”
- “It’s understandable to feel the emotions you’re feeling.”
- DO NOT say invalidating statements like “I understand, but…” “You’ll be fine.” ”There’s no reason to feel that way.” “There’s nothing to worry about.” “It’s not a big deal.” “Why should I respect how you feel if you don’t respect how I feel?” “You are overreacting!” “Calm down.” “Relax.” “Just chill.” “It’s okay.”
- Statements like these may be said with good intentions or may even be true, but regardless of intent they generally shouldn’t be said—especially during intense emotional states. These types of statements are commonly said in our society so they may seem harmless, but they feel dismissive (especially to people with BPD, of all ages). Invalidating statements like these may lead to further outbursts, emotional breakdowns or strains in the parent teen relationship.
- Statements like these may be said with good intentions or may even be true, but regardless of intent they generally shouldn’t be said—especially during intense emotional states. These types of statements are commonly said in our society so they may seem harmless, but they feel dismissive (especially to people with BPD, of all ages). Invalidating statements like these may lead to further outbursts, emotional breakdowns or strains in the parent teen relationship.
- Avoid saying “but.” Instead, replace it with “or” or “and.” The reason for this is because we naturally tend to discredit any words that came before the “but.” (“I think you’re making progress, but…” just doesn’t feel encouraging to teens with BPD, or anyone really—even if you intend it to be). Replacing the “but” could look like:
- “I understand you hate school, and that it’s really hard to wake up in the mornings. It’s honestly hard for me to wake up too. I wish we could lounge around all day together! Unfortunately, though, we both have responsibilities. I have to go to work, and you have to go to school. I need you to get up now so we won’t be late.” INSTEAD OF, “I understand you hate school, but that’s life. Get up now before we’re both late!” The former statement takes longer to say but it’s less likely to result in an intense emotional response whereas the second statement likely would on account of it feeling invalidating and dismissive. Ultimately, in this scenario, being validating would save you both time.
- Keep in mind, if you’ve been unintentionally invalidating in the past—you may have to say multiple validating statements over a longer period of time before their reactions becomes more acceptable overall. Consistency matters A LOT. The more validating you are over time, the more your teen with BPD will come to trust you as a support person and the quicker they will be able to ‘check themselves’ during times of intense emotions.
- Once their emotions have been expressed AND validated—lay out their options in a calm, quiet, monotone voice. This can look like:
- “You’re disappointed that you’re not playing online with your friends right now. That makes sense. Having dinner with the family pales in comparison. I can totally understand that, as a former teenager. However, I would appreciate you being respectful. I need that from you. So you have two options: you can either continue arguing with me about it and you won’t be able to go on after. Which will put a damper on the rest of your night. Or, we can both take a deep breath and you can try your hardest to enjoy this time as a family—and then go online after. Which option would you like to do?”
- “You’re disappointed that you’re not playing online with your friends right now. That makes sense. Having dinner with the family pales in comparison. I can totally understand that, as a former teenager. However, I would appreciate you being respectful. I need that from you. So you have two options: you can either continue arguing with me about it and you won’t be able to go on after. Which will put a damper on the rest of your night. Or, we can both take a deep breath and you can try your hardest to enjoy this time as a family—and then go online after. Which option would you like to do?”
- Address disrespectful behavior after emotions have calmed down and the storm has passed. Maintain the steps above while doing this, so your correction is still validating while also modeling respectful communication. This could look like:
- “I’m glad we sorted all that out. I’m proud of you for telling me how you feel. You were able to regulate your emotions & calm yourself down before the situation got out of control, you should be proud of yourself. I’m thankful you felt safe enough to open up to me. If it’s okay, I’d like to open up to you now before we move on from this. I felt disrespected / hurt / unheard when I was told ________. I’d really appreciate it if next time, those types of words / that tone of voice weren’t used.”
- Thank them for apologizing or for hearing you out. This models effective, two way communication and can help them be better communicators as adults or in their future romantic relationships.
- Make self-improvement & growth feel like a joint family effort by asking them what they think they could do to avoid an escalation next time. This also places the control back in their hands and teaches them that they have a say in their own growth & improvement.
- After they’ve apologized and/or an appropriate consequence has been carried out—allow them and yourself to move on from the situation. Take things one day a time. Progress is never linear, so expect setbacks in your teen with BPD while remaining generally hopeful and optimistic. Take the setbacks in stride. Recovery is not all or nothing.

The Self-Love Workbook
This 103 page digital workbook comes with three different PDFs – full color, a version with no color backgrounds, and a black and white version (to save on printing costs). You get access to all three and you can print whichever one works for you!
DOWNLOAD NOW FOR $10Each .pdf is capable of being filled in digitally. With Adobe on your desktop computer or on an app like XoDo for your phone, you can type your answers into the .pdf and save your progress without ever needing to print it.
What if Teens with BPD are not Willing to Talk or Express Their Feelings?
It’s not uncommon for teens with BPD to not want to talk about their feelings with their parents. If this happens, do not push them as this can backfire and increase intense emotions. Being forced to communicate can also feel patronizing, dismissive and invalidating (which are all common triggers for BPD). Instead, with a neutral voice, say something like, “That’s okay. You don’t need to tell me what’s going on. I’m here to listen, though, if you change your mind. With that said, I do need you to talk to me respectfully.”
If they don’t stop giving you an attitude or lashing out, stop talking and sit quietly. Do not take their words to heart, do not yell at them or let your own emotions build. If it’s safe for them to do so, let them leave the room if they want and give them their space for a couple of minutes or hours—depending on the severity of the episode. Check in on them discreetly and often if you’re worried they’ll do something self-destructive, like cutting.
Once emotions have calmed down and the storm has passed, you can still carry out the last bullet point above. Also keep in mind, that you do not have to know exactly what they’re feeling to be validating—so the tips above that touch on validating statements still hold water even if teens with BPD don’t want to communicate openly.

Validation is key and should be a common occurrence in your household. It’s been proven that teens who grow up in validating environments go on to become happier, more confident and more successful adults. It also builds trust and provides your teen with a sense of safety and love. In essence, it teaches your teen that they matter and ultimately—it will teach them how to validate themselves when they’re older (which is a trait many people with BPD desperately lack and need).
Do NOT leave teens with BPD in the home unattended or let them shut the door to their bedroom, if there’s even a small chance they will act on suicidal ideation. BPD, especially when untreated, does have a high suicide rate; tragically, about 10% of people with BPD die by suicide (that’s not said to put fear in you, but parents of teens with BPD do need to take this statistic seriously). If it’s necessary or if you’re unsure—call a crisis line, a local psychiatric hospital or even the police department for guidance. A hospital visit or a night in the ER may increase the episode in the moment, but that’s always better than the alternative.
Treatment Options for Families of Teens with BPD
If you’re borderline teen is not yet in therapy, find them a therapist as soon as possible. Get them into a dialectical behavior therapy (DBT) group. There are DBT programs available for teens, which can be life changing, whether they have BPD or not. DBT is helpful for various conditions, not just borderline personality disorder. Also consider finding your teen a psychiatrist for an evaluation and/or medication.
If your teen’s symptoms are debilitating and also interfere with their schooling, contact your district’s special education department and request a CSE evaluation and meeting (if you’re in the states, that is—if you’re outside of the states, look into your country’s special education regulations). If your teen is found to be eligible, your school district can provide therapy, various types of special education classes and/or other services during the school day—completely free of charge, on top of the services they receive at home. They may even be able to provide you with regular parent training. My son has received CSE services since kindergarten; his father, stepmother and I have received parent training over the years as well. We wouldn’t be where we are today as a family without these services.
Keep in mind, you may have to fight for these services as some districts are reluctant to qualify students. Consider finding a parent advocate (they are typically free) if you’re having trouble and read up on your state’s individual special education laws. Be informed of your rights as a parent. That’s essential.

As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided.
The saying, “it takes a village to raise a child” cannot be further from the truth when it comes to having a teen with BPD or any other mental disorder. Make your teen with BPD’s treatment a family effort. Built a support system of mental health professionals and child development experts for your family to lean on—do not fight this battle alone. Be actively involved in their treatment. Consider going to family therapy.
Ask your teen’s therapist for referrals to programs that provide in-home services to at-risk youth. My family has utilized these sorts of programs in the past, all for free. Different areas and states will have different programs.
Above all else, get educated on the ins and outs of borderline personality disorder. Learn what your teen is learning in DBT, make the skills a daily part of your lives and/or consider going to your own therapy. Talk openly about your own struggles with mental health with your teen, if you have any experience. This can help build and strengthen your bond. It can make you seem more relatable and safe. As a parent, you should be your teen with BPD’s safe place—the person they know will support and love them no matter what.
Is There Hope For My Borderline Teen?
Yes! There is absolutely hope. This is coming from a woman who did not regularly have the support I detailed above. I lived with a narcissistic parent. I was abused, neglected and was mostly forced to raise myself. When I asked for help or admitted I was feeling suicidal, I was screamed at and told I was an inconvenience. It’s nothing but a miracle that I didn’t die by suicide, given all of my ideation and attempts.
My non-narcissistic parent, while supportive and loving, was sadly not around as much as I needed them because they did not have joint custody of me. They were also being controlled and manipulated by my narcissistic parent. They did not know the severity of the abuse I endured, until years later, because I hid it well from them during our time together.
I say all this to you because if I can get to the point of remission in adulthood, your teen with BPD who is fortunate enough to have a parent reading this post—has a shot, too. Likely a better shot than I did.
(Read ‘How I Overcome Regressions in BPD Recovery’)
Do not give up on your borderline teen. Tell them you love them, often. Reassure them of your love for them, often. Show them your love, often. Tell them you’re proud of them. BPD convinces you that you are unlovable, unworthy, an inconvenience. BPD makes you push loved ones away. It can be debilitating, but there is hope.
BPD Resources
BPD Characters: Read the first 6 chapters of Sadie’s Favorite – an upcoming novel by Sarah Rose, creator of BPD Beautiful.
Get 20% off your first month of BetterHelp. Get matched with a licensed therapist within 48 hours. Subscriptions as low as $65/week, billed every 4 weeks. Cancel anytime.
Manage your BPD symptoms with a printable workbook.
See our recommended list of books about BPD.
Start a Discussion
Parents of teens with BPD! Share your experience in the comments.
Pin This Post
Liked this post? Please help support BPD Beautiful and spread BPD awareness by pinning it on Pinterest.