Psychosis is a broad concept which refers to the experience of losing touch with reality, through symptoms such as hallucinations or delusions. Historically, the existence of psychosis within BPD symptoms has been debated, with only the most recent version of the ICD (America’s official diagnostic manual) including psychoses as part of the listed criteria [1].
How common is psychosis in BPD and what does it look like?
Around 43% of individuals with BPD experience hallucinations [2], the most common type being auditory verbal hallucinations, which are experienced in between 26-54% of people [3]. Auditory hallucinations were often distressing in nature, for example taking the form of someone with higher ‘social power’ than the person with BPD [2]. One study found around half of auditory hallucinations in BPD represented a harsh, punitive parent, highlighting the role of childhood in their manifestation [4]. Other types of hallucinations such as visual, tactile and olfactory can also experienced by individuals with BPD in around 30-33%, 10-30% and 13% of individuals respectively [3].
Delusions, which are fixed beliefs in something that is not considered objectively real, affect around 26% of people with BPD and are on average rated as ‘strong’ on the conviction scale [5]. Delusions are commonly paranoid in nature, for example someone may be convinced everyone is out to get them. One study found paranoia was more likely to emerge when an individual was experiencing difficulties in interpersonal relationships [6]. They may also be manifestations of the pervasive fear of abandonment felt by many individuals with BPD.
Another common psychosis symptom in BPD is dissociation, which is the experience of disconnecting with one’s own emotions, behaviours and identity. Up to 80% of people with BPD experience this and it is usually related to experience of stress, with higher severity for those with a history of childhood maltreatment [7]. For a child experiencing abuse, it may have been beneficial to dissociate from what was going on around them. One specific form of dissociation in BPD is identity confusion, which involves a struggle in understanding who you are as well as the boundaries between yourself and others, which can have a negative impact on interpersonal relationships. This could also contribute to the ‘favourite person‘ dynamic often experienced in BPD.
Why is psychosis considered a ‘pseudo-symptom’ in BPD?
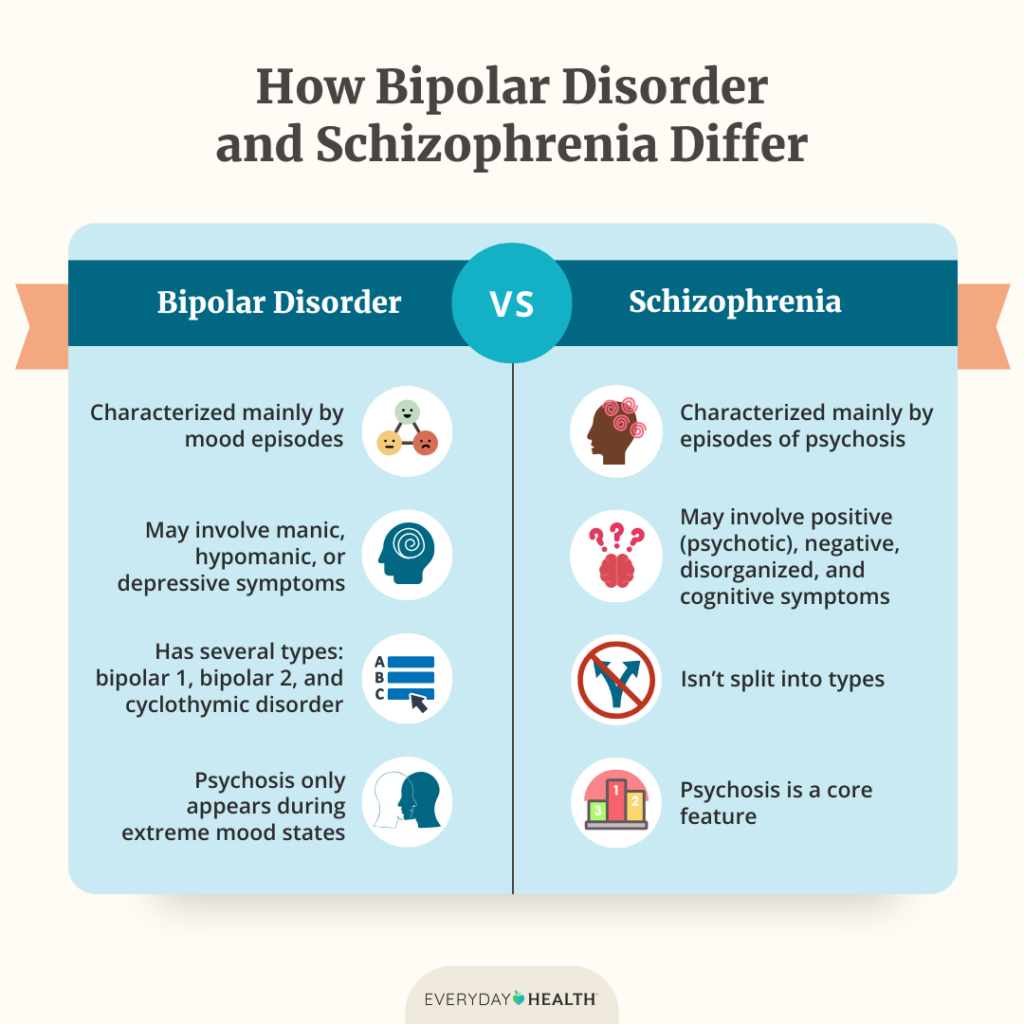
Looking back at the specific definition the ICD-11 gives, “…transient dissociative symptoms or psychotic-like features in situations of high affective arousal” [1], reflects the fact that it is commonly believed psychotic symptoms in BPD are temporary reactions to stress. This is partly due to an unfair comparison with Schizophrenia (a condition in which psychosis is a substantial feature). However, a review of 18 studies comparing both conditions has actually demonstrated that auditory hallucinations in BPD showed more persistence and repetitiveness [11].

As a BetterHelp affiliate, we receive compensation from BetterHelp if you purchase products or services through the links provided.
Delusions in BPD have also been labelled ‘quasi psychotic’ by some i.e. not proper psychosis, however show similar rates of delusion conviction to individuals with Schizophrenia, although patients from the latter group do report more severe preoccupation and distress associated with their beliefs [2]. Hypocritically, the evidence also suggests that just over half of people with Schizophrenia have persistent reoccurring delusions, demonstrating that transience of psychosis can also exist in Schizophrenia, yet their symptoms are not termed ‘quasi psychotic’.
Supporting this, a recent study also found that for a significant portion of individuals with BPD, hallucinations and delusions were present for between 13-18 years prior to the study [5]. This strongly contradicts the perception that psychosis in BPD is always ‘transient’.
Another reason for not taking psychosis as a feature of BPD seriously could be the belief that it is actually a reflection of co-morbid bipolar disorder (present in around 20% of people with BPD), another condition that contains a large psychosis component. However, evidence to support this is mixed [2] and it is very unlikely Bipolar explains all experiences of psychoses in BPD.
How does psychosis in BPD impact the individual?
Studies exploring auditory verbal hallucinations specifically have found that perceiving voices as negative or coming from a higher social rank than oneself predicted depression in BPD youth [8]. As well as this, auditory verbal hallucinations are associated with a co-occurring PTSD disorder and a history of childhood emotional abuse [2]. They have also been found to predict higher suicide risk and readmission to psychiatric hospitals [9] as well as anxiety [10]. Taken together these findings suggest that psychosis in BPD is a marker of more severe BPD.
The review of 18 studies comparing BPD and Schizophrenia also found that individuals with BPD were more likely to perceive their auditory hallucinations as omnipotent and experience more distress and interference in their life as a result of them [11]. This highlights the intense burden that psychosis can place on an individual with BPD and challenges the commonly held belief that psychosis in BPD is not as serious as in other conditions.
How can psychosis be treated in BPD?
For auditory hallucinations specifically CBT can be amended e.g. CBT for voices, which encourages patients to reframe their views about what they hear or CBT-CSE, which focuses on applying strategies to cope with voices. A new method called ‘AVATAR therapy’ also allows individuals to gain control over their hallucinations by building a digital representation of what they have been hearing and has been effective in reducing patient distress. Based on a similar philosophy, ‘Relating therapy’ encourages patients to change their relationship with their voices by being more assertive [12].
For those experiencing dissociation, or a history of childhood trauma, treatment that focuses on traumatic experiences may be of benefit, as both factors contribute to auditory hallucinations in BPD for example. One such approach may be EMDR, which involves the use of eye movement and recollection of traumatic memories and has been shown to reduce the severity of auditory hallucinations in individuals with personality disorders that also have PTSD [13].
Reviews investigating the impact of antipsychotics on psychosis in BPD have found they reduce symptoms [14]. Although many individuals with psychosis are prescribed antipsychotics, any request for such drugs should be discussed with a doctor in detail including weighing up the potential pros and cons of associated side effects.
It is also important to consider evidence that shows adolescence and young adulthood are sensitive periods in which psychosis emerges in BPD [11]. Considering the success of early interventions for psychosis treatments it is of great clinical importance that young individuals with BPD presenting with psychosis are not disregarded as ‘pseudo psychosis’. Sadly, evidence exists to show that this does happen in practice. One study found young people with BPD presenting with their first episode of psychosis did not receive standard care such as the prescription of recommended antipsychotics [15]. This clearly highlights the stigma present in our society.
The Self-Love Workbook
This 103 page digital workbook comes with three different PDFs – full color, a version with no color backgrounds, and a black and white version (to save on printing costs). You get access to all three and you can print whichever one works for you!
DOWNLOAD NOW FOR $10Each .pdf is capable of being filled in digitally. With Adobe on your desktop computer or on an app like XoDo for your phone, you can type your answers into the .pdf and save your progress without ever needing to print it.
Final Thoughts
Based on the current evident base, it is clear that psychosis forms a meaningful part of BPD symptoms and should be thoroughly examined rather than brushed aside in the hopes that it is transient. Referring to these experiences as ‘pseudo’ or ‘quasi’ is demeaning and implies only a certain type of psychosis (such as those associated with Schizophrenia or Bipolar) are worthy of clinical attention. Not only is such a comparison ethically troublesome but in light of psychiatric research preferring dimensional rather than categorical conceptualisations of diagnoses, it is also outdated. Health care professionals should endeavour to be curious about psychosis in BPD patients, particularly in adolescents, where early intervention is of especially high value. In those that psychosis is identified, important questions such as the stability of their psychosis symptoms as well as the impact they have on their day to day function are key.
References
- [1] Source Link
- [2] Source Link
- [3] Source Link
- [4] Source Link
- [5] Source Link
- [6] Source Link
- [7] Source Link
- [8] Source Link
- [9] Source Link
- [10] Source Link
- [11] Source Link
- [12] Source Link
- [13] Source Link
- [14] Source Link
- [15] Source Link
BPD Resources
BPD Characters: Read the first 6 chapters of Sadie’s Favorite – an upcoming novel by Sarah Rose, creator of BPD Beautiful.
Get 20% off your first month of BetterHelp. Get matched with a licensed therapist within 48 hours. Subscriptions as low as $65/week, billed every 4 weeks. Cancel anytime.
Manage your BPD symptoms with a printable workbook.
See our recommended list of books about BPD.
Start a Discussion
Due to the sensitive nature of this post (BPD and Christianity) and the potential for heated debates that could be triggering for some, comments have been turned off.
Pin This Post
Liked this post? Help support BPD Beautiful and spread BPD awareness for ‘BPD Christians’ by pinning it on Pinterest.